Breast cancer is the most common cancer in women. Based on this statistic alone, it’s safe to say that breast cancer requires more attention than your annual gynaecologist check-up.
Survival rates vary worldwide and much of this variation is due to late detection. The later the detection, the later the stage of breast cancer and therefore the lower the survival rate. In most first-world countries, screening, together with improved treatment, results in only one in five women diagnosed with the disease dying of it; in developing countries, it’s estimated that four out five diagnosed women will die of the disease.
How does breast cancer work?
Breast cancer is an uncontrolled growth of the cells in the breast gland, which can spread to other parts of the body via the bloodstream or lymphatic channels. The most important thing to understand, however, is that precursor lesions of breast cancer can be present for as long as 10 to 15 years before a cancer develops. Once breast cancer is established, for two or three years it is only detectable by mammography – even specialists and the woman herself will not be able to detect anything through breast examinations.
What can you do about it?
Practising good breast health and keeping up with technological advances can help women detect abnormalities in their breasts before they become life-threatening. Regular mammography check-ups can help women detect the cancer early, and women also have the option of going for genetic testing for detection of the mutated BRCA gene.
How does a genetic test protect you?
Everyone has BRCA1 and BRCA2 genes. The function of the BRCA genes is to repair cell damage and keep breast cells growing normally; but when these genes contain mutations that are passed from generation to generation, the genes don’t function normally and breast cancer risk increases.
Women carrying mutations of the BRCA genes are about five times more likely to develop breast cancer than those without. In South Africa, the test for the BRCA1 and BRCA2 genes consists of a simple blood sample.
A study suggests that women with a faulty BRCA1 gene typically have a 45 to 90% risk of getting breast cancer during their life, compared to a 12% risk for the average woman. If the results are positive the person can be continuously monitored to ensure early detection of breast cancer if it arises, or they could undergo a preventive mastectomy (as Angelina Jolie did), which will reduce the risk of breast cancer by up to 90%.
Women with an abnormal BRCA1 or BRCA2 gene also have an increased risk of developing ovarian, colon, pancreatic and thyroid cancers, as well as melanoma. However, mutations in BRCA1 and BRCA2 only cause about one in 20 of breast cancers, so just because you don’t have the gene mutation doesn’t mean you’re immune. In fact, 70 – 80% of women who have breast cancer have no family history of the disease.
Breast health management regimes
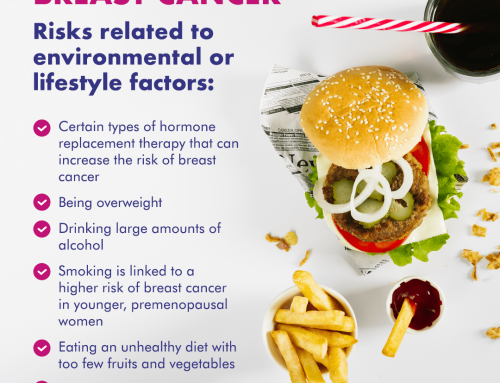
Women, from as young as 20, should have a breast-health management regime in place to ensure the best possibility of early detection. While there is no prevention for breast cancer, it is more likely to occur in women who:
- Have a family history of breast cancer
- Have not had any children or have had children ‘late’ (above 25 years)
- Have not breast-fed
- Had an early first menstruation and late menopause
- Abuse alcohol
- Have a sedentary lifestyle
- Are overweight
- Are on hormonal replacement therapy
Women from the ages 20-39 should know their family history of breast cancer. They should schedule a clinical breast examination by a healthcare professional at least every three years, and should conduct self-breast examinations monthly. Women over 40 should know about the latest advances in breast cancer treatments and technologies. They should have an annual mammogram, arrange for annual clinical breast examination annually and should conduct breast self-examinations monthly.
In addition to regular check-ups and the genetic testing option, we also recommend a three-step approach to breast health.
A life-long breast-care programme should include:
- Breast self-exam
Examine your breasts one week after your period ends. It is easy to do and takes only a few minutes. By knowing what your breasts feel like normally, you will detect changes more easily. Here’s an infographic that shows you how. - Clinical breast exam
Your breast health professional will check your breasts and can demonstrate the proper technique to you. - Mammography
A mammogram is a low dose X-ray of your breasts. It can detect many breast changes that are too small or too deep to feel. Good mammograms are safe, quick and painless.
We all need to be aware of the importance of early detection and good breast health management in general in order to protect South African women from this disease.
By: Professor Justus Apffelstaedt, Associate Professor At University of Stellenbosch and Head of the Breast Clinic At Tygerberg Hospital